 Wayne Ramsay, J.D.
Wayne Ramsay, J.D.
In Part 1 of this essay (8/6/2019)1, I described several reasons the myth of mental illness persists: (1) the effects of repetition of the myth by many people over time, particularly by opinion leaders, (2) disapproval from others for anyone who questions widespread myths, including the myth of mental illness, (3) support for the myth stated by those perceived as experts — in this case psychiatrists, psychologists, and social workers, (4) the desire of some people to avoid personal responsibility for their actions and their lives, (5) there being more comfort in believing a myth than in acknowledging ignorance, and (6) drug companies using huge advertising budgets to perpetuate the myth of mental illness and biological theories of mental illness for the purpose of increasing psychoactive drug sales and maximizing drug industry revenues and profits.
Here in Part 2. I will focus on another of the most important reasons the myth of mental illness persists: the inadequacy of rule of law.
“Rule of law” is a sacred concept in American jurisprudence. On the day she was sworn-in as a U.S. Supreme Court justice, Sonia Sotomayor spoke eloquently about how deeply and sincerely she believes in rule of law. With the exception of civil commitment and involuntary guardianship laws, American courts invalidate laws that fail to put people on notice of what is required or prohibited on the ground they are void for vagueness. An example is Papachristou v. City of Jacksonville wherein a unanimous U.S. Supreme Court overturned the decision of lower courts and declared a Jacksonville, Florida vagrancy ordinance unconstitutionally vague. The Supreme Court said this:
This ordinance is void for vagueness, both in the sense that it “fails to give a person of ordinary intelligence fair notice that his contemplated conduct is forbidden by the statute,” and because it encourages arbitrary and erratic arrests and convictions. Living under rule of law entails various suppositions, one of which is that “[all persons] are entitled to be informed as to what the State commands or forbids.”2
Judged by this standard, all laws authorizing civil commitment for mental illness, or involuntary guardianship (of adults), or other loss of rights because of supposed mental illness, are void for vagueness and unconstitutional because they do not allow people of ordinary intelligence to know in advance what behavior or expression of ideas or outward display of emotions may result in losing their liberty or civil rights because of a “diagnosis” of “mental illness” or mental incapacity.
One might argue the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM) delineates what is and is not a mental disorder, and hence what speech and behavior is and is not allowed, and that therefore the DSM provides the constitutionally required notice of what the state commands or forbids. However, the “Cautionary Statement” at the beginning of DSM-IV-TR explicitly disclaims the manual provides guidance for legal purposes:
It is to be understood that inclusion here, for clinical and research purposes, of a diagnostic category such as Pathological Gambling or Pedophilia does not imply that the condition meets legal or other non-medical criteria for what constitutes mental disease, mental disorder, or mental disability. The clinical and scientific considerations involved in categorization of these conditions as mental disorders may not be wholly relevant to legal judgments, for example, that take into account such issues as individual responsibility, disability determination, and competency.3
An introductory chapter in DSM-5, published in 2013, includes a similar disclaimer titled “Cautionary Statement for Forensic Use of DSM-5”:
...it is important to note that the definition of mental disorder included in DSM-5 was developed to meet the needs of clinicians, public health professionals, and research investigators rather than all of the technical needs of the courts and legal professionals. ... When DSM-5 categories, criteria, and textual descriptions are employed for forensic purposes, there is a risk that diagnostic information will be misused or misunderstood. These dangers arise because of the imperfect fit between the questions of ultimate concern to the law and the information contained in a clinical diagnosis. In most situations, the clinical diagnosis of a DSM-5 mental disorder such as intellectual disability (intellectual developmental disorder), schizophrenia, major neurocognitive disorder, gambling disorder, or pedophilic disorder does not imply that an individual with such a condition meets legal criteria for the presence of a mental disorder or a specified legal standard (e.g., for competence, criminal responsibility, or disability). For the latter, additional information is usually required beyond that contained in the DSM-5 diagnosis ... assignment of a particular diagnosis does not imply a specific level of impairment or disability. ... Nonclinical decision makers should also be cautioned that a diagnosis does not carry any necessary implications regarding the etiology or causes of the individual’s mental disorder or the individual’s degree of control over behaviors that may be associated with the disorder.4
Even if the DSM is nevertheless accepted as a valid standard for legal judgments, it fails to provide the constitutionally required notice of what the state commands and forbids, failure to comply with which may result in forced treatment or loss of liberty, because the DSM does not state which supposed disorders justify involuntary commitment, or loss of civil rights, and which do not.
In The Manufacture of Madness in 1970, psychiatry professor Thomas S. Szasz, M.D., said, “psychiatry shows an unmistakable tendency to interpret all kinds of deviant or unusual behavior as mental illness.”5 When Dr. Szasz wrote those words, homosexuality was an example. Would it have been appropriate to subject all homosexuals to involuntary treatment prior to the American Psychiatric Association’s vote in 1973 to de-designate homosexuality as a mental disorder? The DSM-II, published in 1968, said homosexuality was a mental disorder,6 but it did not say all homosexuals should be treated involuntarily if they refused treatment for their homosexuality. However, it probably happened to homosexual adolescents whose parents were upset by their homosexuality. Some of those adolescents may even have been lobotomized (yes: lobotomized) as treatment for their homosexuality: In Psychosurgery—Damaging the Brain to Save the Mind in 1992, Joann Ellison Rodgers of The John Hopkins Medical Institutions says in the middle of the 20th Century:
Rapists, pedophiles, homosexuals, exhibitionists, and transvestites were all candidates for lobotomies. ... Many lobotomies, for example, were performed on the institutionalized mentally ill to stop or limit ‘bizarre’ sexual behavior, which at that time meant masturbation, homosexuality, and for women, almost any overt desire for sexual release.
Similarly, in 2005 Emad N. Eskandar, M.D., G. Rees Cosgrove, M.D., and Scott L. Rauch, M.D., of Massachusetts General Hospital and Harvard Medical School said:
Psychiatric neurosurgery was first introduced as a treatment for severe mental illness by Egas Moniz in 1936. ... despite a lack of objective therapeutic benefit, psychiatric neurosurgery was enthusiastically adopted by practitioners of the day. At the height of enthusiasm, psychiatric neurosurgery was recommended for curing or ameliorating schizophrenia, depression, homosexuality, childhood behavior disorders, criminal behavior and uncontrolled violence.7
Lobotomizing people as treatment for masturbation, homosexuality, or normal heterosexual desire is an example of harm caused by psychiatric “diagnosis” that is based on deviance from cultural norms or values rather than demonstrated biological abnormality. It is also an example of why I call psychiatry evil.
I have uncovered no 21st Century reports of involuntary psychosurgery, but brain-damaging “medication” and electroshock are given to people over their objection every day in the U.S.A., either of which is capable of inflicting brain damage as severe as occurs with psychosurgery.
LOBOTOMY AS TREATMENT FOR HOMOSEXUALITY?
People are committed involuntary to mental hospitals every day in the U.S.A. because they have “suicidal ideation” despite the fact that neither the DSM nor civil commitment laws put people on notice they are allowed to think about some things but not other things. Where is it written, even in the DSM, that Americans are not permitted to even think about ending their own lives—and that, if they do, loss of liberty may be the consequence?
This leaves aside the equally important question of whether the there is a right to freedom of thought under U.S.A.’s First Amendment (made applicable to the states by the Fourteenth Amendment), similar state constitutional provisions (e.g., Article 1, Section 8 of the Texas Constitution), or constitutional provisions in other countries, that should take precedence over psychiatry’s supposedly diagnostic (but actually only descriptive) classification system and the State’s statutory involuntary commitment criteria.
It should be obvious that one of the purposes of the DSM is to allow mental health professionals to bill health care insurance companies and government programs such as Medicare and Medicaid for virtually anything (which is one reason health care insurance premiums are exorbitant, and one reason health care and health care insurance are bankrupting the U.S. government and bankrupts many Americans). Much normal human thinking and behavior at least arguably falls within a category of mental disorder in the DSM. The supposedly diagnostic (but actually only descriptive) criteria in the DSM are so broad that many commentators and critics have correctly said there probably is no human being alive who falls within none of the DSM’s various categories of mental disorder, and most people meet the criteria for several psychiatric diagnoses simultaneously. For example, “In court testimony, under oath, Jay Katz, a professor of psychiatry at Yale, admitted that ‘If you look at DSM-III you can classify all of us under one rubric or another of mental disorder’”.8 In his book The Hyperactivity Hoax, board-certified neurologist and psychiatrist Sydney Walker III, M.D., said:
The other major flaw of DSM, related to the first, is that it labels virtually everything as some type of disorder. Thus, a child who sees a DSM-oriented doctor is almost assured of a psychiatric label and a prescription, even if the child is perfectly fine.9
According to Marcia Angell, M.D., Senior Lecturer in Social Medicine at Harvard Medical School and former editor-in-chief of The New England Journal of Medicine, in her endorsement on the dust cover of Dr. Allen Frances’ book, Saving Normal, Dr. Frances “was once the most influential psychiatrist in the country, as head of the task force that compiled the last [fourth] edition of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM)”. Yet even this highly esteemed psychiatrist, Dr. Frances, says he “met many other friends working on DSM-5 who were similarly excited by their pet innovations and soon discovered that I personally qualified for many of the new disorders that were being suggested by them for inclusion for DSM-5.”10 Dr. Frances cites “a study that found 83 percent of kids qualify for mental disorder diagnosis by the time they are twenty-one.”11 In 2013 in their book Mad Science: Psychiatric Coercion, Diagnosis, and Drugs, three American professors of social work and social welfare said:
According to the latest American Psychiatric Association methods of diagnosing mental illness, nearly one hundred million people, 25 to 30 percent of the US population, have a mental illness during any one year, and half of the population will have a mental illness during their lifetime.12
Similarly, in 2011 Dr. Vernon Coleman, a British physician, wrote that “diagnostic symptomotology is so vague and far reaching that I could, without much difficulty, find some definable mental illness in every person in the UK.”13
In 1997 in Whores of the Court: The Fraud of Psychiatric Testimony and the Rape of American Justice, Boston University psychology professor Margaret A. Hagen, Ph.D., said:
The newest (1994) Diagnostic and Statistical Manual of Mental Disorders provides the civil litigant with literally hundreds of possible disorders, each neatly laid out with the necessary symptoms. It is hard to imagine that anyone could live in today’s society and not be diagnosed with at least one of these many disorders.14
THE DSM LABELS VIRTUALLY EVERYTHING AS SOME TYPE OF DISORDER
DSM-5 broadens the categories of mental disorder even more than DSM-III, DSM-IV or DSM-IV-TR. According to Dusan Kecmanovic, professor of psychiatry and political psychology at Sarajevo University, “it will be difficult to be normal after the publication of DSM-5.”15 (Americans should keep this in mind when considering laws to keep guns out of the hands of “the mentally ill”: Since nearly everyone qualifies as mentally ill under current criteria, such laws could in application be a de facto repeal of the Second Amendment.) In her book, The Trouble With Drug Companies, Dr. Marcia Angell says, “few psychiatric disorders have objective criteria for diagnosis”.16 Actually, none do. The vague, unreliable, unpredictable, and invalid nature psychiatric diagnosis enables and encourages arbitrary “diagnosis” and arbitrary involuntary treatment. That violates the constitutional standard stated by the Supreme Court in Papachristou.
The constitutional law requirement that government must tell you what is and is not allowed before it may do anything to you as a consequence of your failure to act as expected is only fair. That’s why the U.S. Supreme Court has declared it to be constitutionally required.
There is, however, a problem with this constitutional requirement, or said another way, there is a problem with rule of law: We can’t always anticipate and articulate, in advance, everything a human being might possibly say or do that other human beings, upon being made aware of it, will consider unacceptable.
This epiphany came to me in 1992 when I was sitting at a table in a restaurant in Manhattan with the woman I was dating at the time. Our table was located next to a window on the other side of which was a sidewalk. A man who looked like he was homeless put his face very close to the window as he stared at us, pointed at us, made funny faces, and did an odd sort of dance. His behavior was distracting and inappropriate, but how would one write a law prohibiting what he was doing?: Don’t look into or get too close to restaurant windows? Don’t point at people? Don’t make funny faces? Don’t dance on the sidewalk?
Similarly, I once saw a man sleeping on the floor in a hotel corridor with his face against a dirty carpet. At first I thought he might be dead, but after several seconds of observation I could see he was breathing. I advised the hotel front desk clerk who roused the man and told him he couldn’t sleep there and told him to go sleep in his hotel room.
The next day in a Subway Sandwich Shop a patron who looked like he was homeless began singing loudly and vastly off-pitch along with the music playing on speakers in the ceiling of the shop, disturbing everyone in the shop.
Examples abound in the evidence introduced at involuntary commitment and involuntary guardianship hearings. After I think I’ve heard and seen everything, the behavior or ideas of a proposed patient in an involuntary commitment for supposed mental illness or of the proposed adult ward in an involuntary guardianship trial confronts me with yet another example of unacceptable thinking or behavior I wouldn’t have thought of had I been given the job of writing a state’s criminal code and other laws. It is largely because of this difficulty that we have the concept of mental illness.
Sociologist Thomas Scheff has defined mental illness as “residual rule-breaking”: “After crime,” wrote two of his critics, “perversion, drunkenness, bad manners, there are always those diverse grab-bag violations for which the culture has no explicit label—the ‘residual rules’ broken by those deemed mentally ill.”17 The concept of mental illness allows us, as a society, to impose sanctions, that is, punishment (called “therapy”) on law-abiding people who fail to live in accordance with our expectations about what conduct people should and should not engage in, and what beliefs or thoughts people should or should not express. As psychiatry professor Thomas Szasz said in 1994, “when I grew up in Hungary—1920s, 1930s—it was very, very clear that psychiatry was essentially a jail function. There were blue coated policemen and white coated policemen.”18 In "Mental Illness as Brain Disease: A Brief History Lesson," Dr. Szasz says “The contention that mental illness is brain disease is as old as psychiatry itself: it is an integral part of the grand lie that psychiatry is a branch of medicine and healing, when in fact it is a branch of the law and social control.”19
Similarly, in 2011 three authors including psychology professor Mark Rapley and psychiatrist Joanna Moncrieff call psychiatry “the enterprise of policing human conduct”.20
British psychiatrist Suman Fernando says “psychiatry...from the very beginning...has been concerned with social control.”21
In Madness—A Brief History, Roy Porter, Professor of the Social History of Medicine at the University College, London says “To many the psychiatrist seemed to have been reduced to acting as society’s policeman or gatekeeper, protecting it from the insane.”22
The role of psychiatrists as police is also underscored by the subtitle of Louise Armstrong’s book And They Call It Help—The Psychiatric Policing of America’s Children.23
Blue-coated police enforce written laws. White coated police—psychiatrists and those who work with them—enforce unwritten laws prohibiting thinking and behavior we either didn’t think to write a law against or choose not to (for reasons discussed below) or for which we just can’t find the right words (like my above examples). Psychiatry’s roles as (1) part of the medical profession and (2) de facto police who enforce society’s unwritten laws are obfuscated and confused, resulting in violators of society’s unwritten laws not having the benefit of the protections that exist in criminal law. Violating society’s unwritten laws is called mental illness or mental disorder. The punishment is imprisonment called involuntary hospitalization and psychological and physical misery and brain damage caused by “involuntary medication” or involuntary electroconvulsive “therapy”.
Oddly, violators of our unwritten laws tend to be punished more harshly than those who violate our written laws: Would anyone advocate drug or electroshock induced brain damage as punishment for bank robbery or even murder?
New York (or whatever state’s) Penal Code
Punishment for a Class A misdemeanor shall be involuntary administration of a neurotoxic medication until brain damage and permanent neurological disease or disability including uncontrollable muscle movement (dyskinesia) is achieved.
Such a law would probably be declared a violation of the U.S. Constitution’s Eighth Amendment prohibition of cruel or unusual punishment. However, inflicting exactly this on a person becomes acceptable when administered as “therapy” for “mental illness,” and it is commonplace, even though mental “illness,” like crime, is nothing more than violating society’s (other people’s) rules.
Our current approach of calling prohibited thinking or behavior “mental illness” circumvents the difficult task of defining, in advance, what is and is not permitted, and it permits us to impose especially severe punishments. It is easier to call people mentally ill and incarcerate and punish them with supposed treatment for their supposed mental illness than it is to anticipate everything people might do that is unacceptable and enact laws prohibiting the behavior.
PSYCHIATRISTS AND THEIR CO-WORKERS ARE
WHITE-COATED POLICE WHO ENFORCE SOCIETY’S UNWRITTEN LAWS
Sometimes belief in mental illness, or a pretense there is such a thing as mental illness, is the only way we can impose sanctions for disliked speech or behavior because, if we were to write laws clearly describing what is prohibited, it would be obvious we are violating the constitutional rights of the accused with such laws. For example, people are often forced into psychiatric “treatment”, including involuntary hospitalization, because of what they say rather than because of what they do. Does this violate the First Amendment guarantee of freedom of speech? Does the First Amendment protect only speech other people consider sane or rational?
Refusing to speak when other people think you should is another example. In 2011, I was an observer at an involuntary commitment hearing of a man whose “Selective Mutism” (rarely saying a word to anyone, DSM-IV-TR diagnosis 313.23)24 was his main supposed symptom of supposed mental illness, and at that hearing (after expiration of the time he could be held on a criminal charge) he was involuntarily committed to Kerrville State Hospital. In 1977, in Wooley v. Maynard, the U.S. Supreme Court said, “the right of freedom of thought protected by the First Amendment against state action includes both the right to speak freely and the right to refrain from speaking at all.”25 Texas Jurisprudence, a legal encyclopedia, says, “Liberty of silence is included by the guarantee of liberty of speech.”26 Because it would be unconstitutional, nobody is going to write a law saying you must speak with people. Nevertheless, engaging in normal conversation with those around you is an expectation nearly everyone has. Therefore, mutism or selective mutism can become “mental illness” motivating involuntary “treatment” and did in this case despite the constitutional right to, in the U.S. Supreme Court’s words, “refrain from speaking at all.” It is possible to incarcerate a person because he exercises a constitutional right such as refusing to talk if the ostensible or supposed reason is “mental illness” rather than the constitutionally protected action or inaction.
We could enact criminal laws against mutism, or unconventional religious or philosophical beliefs, or converting to a religion your family abhors, or loudly expressing nonreligious beliefs most people disagree with, or being grandiose or obnoxious, or revealing oneself to be excessively unhappy (“depressed”), or talking aloud to oneself with others present, or admitting to thinking about suicide, or attempting suicide. We don’t, because writing such laws wouldn’t seem right. In many cases such laws would be an admission of how narrow-minded, intolerant, authoritarian, and even despotic we sometimes are, including in nations like the United States of America where freedom is frequently touted as the reason for American patriotism. Frequently, such laws would be impossible to reconcile with America’s First Amendment guarantee of freedom in thought and expression or similar guarantees in other democracies and Article 19 of the United Nations Universal Declaration of Human Rights adopted by the United Nations General Assembly in Paris on December 10, 1948:
Everyone has the right to freedom of opinion and expression; this right includes freedom to hold opinions without interference and to seek, receive and impart information and ideas through any media...
State and federal laws authorizing civil commitment for mental illness in the United States of America and other nations routinely violate this right to freedom of opinion and expression. Freedom of thought, opinion, and expression is respected in the U.S.A. if a person thinks Jesus is the Son of God but not if he thinks he is the Son of God, or if he thinks others are persecuting him (and others disagree), or if he thinks his life is not worth living (and others disagree), or if he has other thoughts other people consider crazy or bothersome. As psychiatry professor Thomas Szasz wrote in 1973: “If you talk to God, you are praying; If God talks to you, you have schizophrenia.”27 We on the Western side of what was once (prior to the breakup of the USSR) called the Iron Curtain like to think of ourselves as freedom-loving people who uphold human rights. The concept of mental illness permits us to violate our professed values about freedom and disregard the principal of rule of law without admitting to ourselves this is what we are doing. It permits us to violate what the American Declaration of Independence of July 4, 1776 says are the God-given and unalienable rights of all men (and women): “...that all men are created equal, that they are endowed by their Creator with certain unalienable Rights, that among these are Life, Liberty, and the pursuit of Happiness.” The myth of mental illness permits us to deprive law-abiding people of their supposedly unalienable right to liberty and pursuit of happiness, and because of fatal effects of psychiatric “treatment” such as sudden death caused by neuroleptic “medications” effect on the heart, or neuroleptic malignant syndrome, or electroshock, or physical restraint (causing asphyxiation), sometimes even their right to life, by pretending we are “treating them for their mental illness.” Ron Leifer, M.D., a psychiatrist, said it well in 2000:
The problem is that society demands a greater degree of social control than law allows. The public wants to be protected from unconventional, threatening, and dangerous behavior. There is, thus, a public mandate for a covert form of social control which supplements rule of law. Medical-coercive psychiatry, in alliance with the state, performs this function disguised as medical diagnosis and treatment. ... involuntary, coercive psychiatry serves society by providing a supplemental form of social control which, because it is covert or disguised, preserves our national pride by giving us the appearance of being a nation of free individuals under law. On the other hand, when the covert is exposed it can be seen to violate the honored values on which this nation was founded.28
An example that was prominently featured in news reports in New York City in 1987 was the use of the concept of mental illness to get homeless people off the streets and out of the public parks of the City. A New York Times article called it “a Koch administration program to involuntarily hospitalize severely mentally ill homeless people living on city streets.”29 Rather than admit the real motive was getting rid of these people whose presence was irritating to other people, New York City Mayor Ed Koch asserted the purpose was to get them “hospitalized” (involuntarily, of course) for allegedly needed “mental health” treatment. It was a classic case of oppression disguised as benefaction. New York lawmakers could have created a law making it illegal to be homeless or to sleep on park benches, sidewalks, or in subway stations and swept homeless people into detention facilities of some kind. But they couldn’t or didn’t want to accept the moral implications of such a choice and therefore preferred to use mental illness as an excuse to justify incarcerating homeless people. This was intellectually dishonest, because the real reason was disapproval of or annoyance with homeless people, and because imprisonment does not become benign merely because it is called hospitalization.
Even if it were possible to anticipate everything people might do that we as a society want to prohibit, and even if we didn’t care if writing such laws clearly and explicitly reveals we are violating human and constitutional rights with such laws, in many cases it would be impossible to write a statute that would prohibit the behavior we want to prohibit without encompassing other behavior we do not want to prohibit. An example is crying in public. A person who cries in public too often, or for reasons with which few others sympathize, or for reasons others don’t understand, bothers other people. Few would advocate making it illegal to cry in public, because there are circumstances in which most people think crying in public is understandable and acceptable and shouldn’t be prohibited. People are expected to intuitively know when it is okay to cry in public and when it isn’t. A person who cries in public for reasons with which others are unsympathetic or at times others dislike, or more often and more loudly than other people think is appropriate, is breaking a residual rule of behavior, that is, a rule that isn’t written anywhere but which people are nevertheless expected to know about and abide by. Violating this unwritten expectation may result in punishment called involuntary psychiatric treatment, including involuntary “hospitalization” for major depressive disorder or some other supposed diagnosis. How and when and how loudly to express one’s anger, even verbally and without threatening others with physical harm, is also the subject of residual rules of conduct the violation of which might result in involuntary psychiatric “treatment”, including involuntary “hospitalization” or an involuntary outpatient commitment court order compelling a person living in his own house or apartment to appear at a clinic for bi-weekly or monthly injections of a long-acting drug intended to treat a supposed mental illness such as inappropriately expressed anger.
THE CONCEPT OF MENTAL ILLNESS PERMITS US TO VIOLATE OUR PROFESSED VALUES ABOUT FREEDOM AND RULE OF LAW WITHOUT ADMITTING TO OURSELVES THIS IS WHAT WE ARE DOING
In a letter dated October 14, 2009, I proposed the above ideas to retired psychiatry professor Thomas S. Szasz, who I had shortly before visited in his home town of Manlius, New York:
I believe the reason the myth of mental illness continues is not only or even mainly because people do not understand its scientific invalidity, although that is of course a factor. I believe one of the most important reasons the concept of mental illness continues to be accepted legally and otherwise is it is impossible to write into criminal codes and other laws all commonly held expectations of behavior—and people’s desire to enforce these unwritten expectations. Mental illness is the rationalization used to punish people who violate unwritten rules—with punishment called involuntary hospitalization, and with torture inflicted as punishment but called treatment for the supposed but actually nonexistent “mental illness”. ... I think overcoming this problem is an important challenge facing people like you and me who want America and other nations to be governed by rule of law rather than arbitrary after-the-fact determinations of what behavior was right or wrong.
With my above letter I gave Dr. Szasz a tape recording I had made of the speeches including his own at the Thomas S. Szasz Tribute Dinner I had attended in Manhattan in 1990. Dr. Szasz’s reply in an e-mail on October 19, 2009 was “Dear Mr. Ramsay, Many thanks for the tape - and your letter, with which I agree completely. Marginal rule violation and its punishment is the name of the game. Best wishes, Thomas Szasz”
MARGINAL RULE VIOLATION AND ITS PUNISHMENT IS THE NAME OF THE GAME
We as a society and as citizens of democracies would be more honest if we discard the myth of mental illness, repeal our civil commitment laws, and in their place enact a criminal law that openly acknowledges legislators are unable to anticipate and write a law against every act that should be prohibited. Such a law might be titled “Criminal Conduct NOS." It seems the majority of psychiatric diagnoses in involuntary civil commitment for mental illness I have seen end with the letters NOS, e.g., Personality Disorder NOS or Psychotic Disorder NOS. In his book Hippocrates Cried: The Decline of American Psychiatry in 2013 psychiatrist Michael Alan Taylor, M.D., says “upward of a third of psychiatric patients end up being given the label NOS (Not Otherwise Specified).”30 Even with the ever-increasing number of supposedly diagnostic categories with each new edition of the American Psychiatric Association’s DSM, resulting in each edition being a bigger book with more diagnoses (or descriptions) than the last, psychiatrists continue to find it necessary to use “NOS” diagnoses. If we are going to incarcerate people on the basis of a supposed diagnosis ending with the letters NOS, why not have a criminal law with a name ending in NOS that does the same thing? Criminal Conduct NOS might be defined as “an act not mentioned in this Penal Code but which the defendant knew or if he was a reasonable person of ordinary intelligence would have known he should not have performed.” Replacing civil commitment law with a criminal or penal code provision such as Criminal Conduct NOS would represent a constriction of the power of families and government to incarcerate and punish people for (otherwise) lawful but bothersome behavior, or what Dr. Szasz called marginal rule violation, compared with today’s laws authorizing civil commitment for supposed mental illness, for these reasons: To obtain a conviction for Criminal Conduct NOS, the prosecution would be required to prove the defendant was guilty of specific past act rather than allowing imprisonment (called involuntary “hospitalization”) and corporal punishment and psychological torture (called involuntary “medication” or involuntary electroshock) for an alleged, arbitrarily and often vaguely defined state of mind such as depression or schizophrenia or bipolar or personality disorder, or predicted future conduct—“dangerousness.” The “clear and convincing” standard of proof permitted by the U.S. Supreme Court in civil commitment for supposed mental illness in Addington v. Texas31 and employed in many states of the U.S.A., would be replaced with the more stringent standard of proof “beyond a reasonable doubt” that applies in criminal cases. Most Americans have a right to trial by jury in civil commitment for mental illness, but many do not. If civil commitment laws are repealed and Criminal Conduct NOS is added to each state’s criminal code, the defendant’s right to trial by jury would be respected to the same extent it is in other criminal cases, because legislators and judges would no longer be playing word games or employing deceptive semantics to avoid respecting defendants’ constitutional rights, including the right to trial by jury, by calling the proceedings “civil” or “special” rather than criminal. The judge or jury would be required to find the defendant not only did the act alleged but also at the time knew what he did was wrong or that a reasonable person of ordinary intelligence would have known what he did was wrong. To avoid convicting a person who lacked the mental capacity of a reasonable person of ordinary intelligence of a “criminal” offense, the judge or jury would need to be empowered to find the defendant did the act alleged, that a reasonable person of ordinary intelligence would have known the act was wrong, but that the defendant lacked the mental capacity of a reasonable person of ordinary intelligence, withhold adjudication of a “criminal” offense, and sentence the defendant to a type of incarceration or program deemed educational or therapeutic.
Some will object to this approach because it does not allow intervention to prevent future acts. My response is we can’t predict a person’s future conduct reliably enough to justify incarceration as a preventive measure. In the words of a clergyman whose Sunday sermon I saw on C-Span on January 1, 2012, “The only evidence of what a person will do in the future is their record of what they have done in the past.”32 A person’s future conduct cannot be proved by any burden of proof, not even “preponderance of the evidence”, unless perhaps he says he is going to do something, or he has a long history of similar acts in the past.33
Substituting a criminal law titled Criminal Conduct NOS for current civil commitment law is only a partial solution, because sometimes people’s behavior is bothersome but does not justify criminal prosecution, including Criminal Conduct NOS. Enforcement of private property rights that give property owners authority regarding what can be done on their property may be the best solution in some situations.
Because there is no credible evidence of any so-called mental illness being caused by biological abnormality, so-called mental illness is definable only as thinking or behavior that is considered unacceptable. Without a biological abnormality proved to be the cause of the behavior or supposed symptoms, a supposed mental illness does not qualify as true illness or as true disease. The word “mental” implies non-physical: A person can no more have “mental illness” than he can have mental cancer. It is possible to have brain cancer but not mental cancer. For similar reasons, it is possible to have a brain disease but not a mental disease. Likewise, it is no more possible to have a “mental” illness than it is possible to have a “religious illness” or a “political illness.” Mental illness exists only as a concept in the minds of people who believe in mental illness. Involuntary psychiatric “therapy” is punishment for thinking or behavior people dislike, not health care as people like to think and as legislators and judges assume. If the so-called professionals in what we call mental health allowed themselves to use only the term brain disease (not “mental illness”) and refused to believe a brain disease is present unless true physical, biological (not merely mental, emotional, or behavioral) evidence is found, most if not all psychiatric and psychological “diagnosis” (confusing values with health) would cease. But then, as psychiatrist Ronald Leifer pointed out (above), we as a society would be stuck with rule of law, and “the public will be deprived of an extra-legal means of maintaining domestic tranquility."34
Belief in mental illness continues for all of the above reasons, none of which are valid from a logical or scientific or legal and constitutional standpoint.
1Wayne Ramsay, J.D., “Why the Myth of Mental Illness Lives On (Pt. 1), ISEPP Bulletin July 2019, https://psychintegrity.org/why-the-myth-of-mental-illness-lives-on-part-1
2Papachristou v. City of Jacksonville, 405 U.S. 156 at 162 (1972), citations omitted
3Diagnostic and Stastical Manual of Mental Disorders, 4th edition, text revision (DSM-IV-TR, American Psychiatric Association 2000), p. xxxvii
4Diagnostic and Stastical Manual of Mental Disorders, 5th edition (DSM-5, American Psychiatric Association 2013), p. 25
5Thomas S. Szasz, M.D., The Manufacture of Madness (Harper & Row 1970), p. 68)
6Diagnostic & Statistical Manual of Mental Disorders — Second Edition (American Psychiatric Association 1968), p. 44
7Emad N. Eskandar, M.D., G. Rees Cosgrove, M.D., and Scott L. Rauch, M.D., “Psychiatric Neurosurgery”, neurosurgery.mgh.harvard.edu, accessed February 5, 2014, underline added
8Prof. Jay Katz, quoted in Thomas Szasz, Insanity—The Idea and It’s Consequences (Syracuse University Press 1997), p. 57
9Sydney Walker III, M.D., The Hyperactivity Hoax (St. Martin’s Press 1998), p. 23. Italics are Dr. Walker’s.
10Allen Frances, M.D., Saving Normal—An Insider’s Revolt Against Out-of-Control Psychiatric Diagnosis, DSM-5, Big Pharma, and the Medicalization of Ordinary Life (HarperCollins 2013), p. xvii
11Id., p. 177: Journal of American Academy of Child and Adolescent Psychiatry: “Cumulative Prevalence of Psychiatric Disorders by Young Adulthood: A Prospective Cohort Analysis from the Great Smoky Mountains Study”, Vol. 50, No. 3, (2011) pp. 252-261, available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3049293/
12Stuart A. Kirk, et al., Mad Science: Psychiatric Coercion, Diagnosis, and Drugs (Transaction Publishers 2013, p. vii
13Vernon Coleman, MBChB, D.Sc.(hon), Do Doctors and Nurses Kill More People Than Cancer?, (European Medical Journal 2011), p. 32
14Margaret A. Hagen, Ph.D, Whores of the Court: The Fraud of Psychiatric Testimony and the Rape of American Justice (ReganBooks 1997), p. 250
15Dusan Kecmanovic ,“DSM-5: The More It Changes The More It Is the Same”, Psychiatria Danubina, 2013; Vol. 25, No. 2, pp. 94-96
16Marcia Angell, M.D., The Truth About Drug Companies—How They Deceive Us and What To Do About It (Random House 2005), p. 88
17Rael Jean Isaac & Virginia C. Armat, Madness in the Streets (Free Press/Macmillan 1990), p. 49
18“Thomas Szasz on Socialism in Health Care”, https://www.youtube.com/watch?v=FC9r3Gs8XuU, at 1:24:42
19Thomas Szasz, M.D., “Mental Illness as Brain Disease: A Brief History Lesson”, http://www.szasz.com/freeman13.html, accessed September 16, 2020
20Mark Rapley, et al., Medicalizing Misery, Palgrave Macmillan 2011, p. 4
21Id., p. 50
22Roy Porter, Madness—A Brief History, (Oxford University Press 2002), p. 186
23Louise Armstrong, And They Call It Help—The Psychiatric Policing of America’s Children (Addison-Wesley Pub. Co. 1993).
24DSM-IV-TR diagnosis code 313.23 appears on p. 125
25Wooley v. Maynard, 430 U.S. 705 at 714 (1977)
269 Tex.Jur. Constitutional Law §91, p. 525
27Thomas Szasz, M.D., The Second Sin (Anchor/Doubleday 1973), p. 113
28Ron Leifer, M.D., “A Critique of Psychiatry and an Invitation to Dialogue”, Ethical Human Science and Services, December 27, 2000, available at www.critpsynet.freeuk.com/critique.htm
29Josh Barbanel, “New York Ordered to Find Care for Homeless Woman”, The New York Times, November 25, 1987, p. B3
30Michael Alan Taylor, M.D., Hippocrates Cried: The Decline of American Psychiatry (Oxford University Press 2013), p. 39
31Addington v. Texas, 441 U.S. 418 (1979)
32Rev. Bill Tvedt, Jubilee Family Church, Oskaloosa, Iowa
33See Is Involuntary Commitment for “Mental Illness” or “Dangerousness” a Violation of Substantive Due Process?, www.wayneramsay.com/due-process.htm
34Ron Leifer, M.D., “A Critique of Psychiatry and an Invitation to Dialogue”, Ethical Human Science and Services, December 27, 2000, www.critpsynet.freeuk.com/critique.htm, accessed March 9, 2013.

 Last year's conference addressed the question: "How did we allow biological psychiatry take a strangle hold of the struggles and diversity of humanity?"
Last year's conference addressed the question: "How did we allow biological psychiatry take a strangle hold of the struggles and diversity of humanity?"  Dr. Johnstone is a consultant clinical psychologist, author of Users and Abusers of Psychiatry (2nd edition, Routledge, 2000) and co-editor of Formulation in Psychology and Psychotherapy: Making Sense of People’s Problems (2nd edition, Routledge, 2013) and A Straight-Talking Guide to Psychiatric Diagnosis (PCCS Books, 2014), along with a number of other chapters and articles taking a critical perspective on mental health theory and practice.
Dr. Johnstone is a consultant clinical psychologist, author of Users and Abusers of Psychiatry (2nd edition, Routledge, 2000) and co-editor of Formulation in Psychology and Psychotherapy: Making Sense of People’s Problems (2nd edition, Routledge, 2013) and A Straight-Talking Guide to Psychiatric Diagnosis (PCCS Books, 2014), along with a number of other chapters and articles taking a critical perspective on mental health theory and practice.  Dr. Yakushko is a licensed psychologist, practicing clinician, and a professor in the Clinical Psychology program at Pacifica Graduate Institute (Carpinteria, CA). Her initial scholarship focused on xenophobia and such global concerns as trafficking and gender violence. Her recent work seeks to examine the impact of historical forms of scientific ideologies, such as the eugenics movement, on past and contemporary discipline/practice of psychology and other mental health fields. In addition, she traces eugenics based sciences/scientism to such contemporary phenomena as "race realism" (dominant in promotion of White supremacy), "evolutionary psychology" (central to justifications in the "manosphere" and related online misogyny groups), and "positive psychology" (highly popularized psychology efforts to promote ahistorical, biologized and social/emotional control-based views of humanity). She is an author of over 60 peer reviewed articles and book chapters. Her recent books include Modern Day Xenophobia (Palgrave, 2018) and Scientific Pollyannaism (Palgrave, 2019). Her upcoming publication entitled "Shameful Sciences!": Eugenics and Its Evolution in American Psychology is scheduled to be released in 2022. She is a Fellow of the American Psychological Association, a Board Member of APA's Division 39 (Psychoanalysis), and the recipient of the Leadership Award of the Committee on Women in Psychology (APA) in 2021.
Dr. Yakushko is a licensed psychologist, practicing clinician, and a professor in the Clinical Psychology program at Pacifica Graduate Institute (Carpinteria, CA). Her initial scholarship focused on xenophobia and such global concerns as trafficking and gender violence. Her recent work seeks to examine the impact of historical forms of scientific ideologies, such as the eugenics movement, on past and contemporary discipline/practice of psychology and other mental health fields. In addition, she traces eugenics based sciences/scientism to such contemporary phenomena as "race realism" (dominant in promotion of White supremacy), "evolutionary psychology" (central to justifications in the "manosphere" and related online misogyny groups), and "positive psychology" (highly popularized psychology efforts to promote ahistorical, biologized and social/emotional control-based views of humanity). She is an author of over 60 peer reviewed articles and book chapters. Her recent books include Modern Day Xenophobia (Palgrave, 2018) and Scientific Pollyannaism (Palgrave, 2019). Her upcoming publication entitled "Shameful Sciences!": Eugenics and Its Evolution in American Psychology is scheduled to be released in 2022. She is a Fellow of the American Psychological Association, a Board Member of APA's Division 39 (Psychoanalysis), and the recipient of the Leadership Award of the Committee on Women in Psychology (APA) in 2021.  Dr. Walker is a liberation psychologist, writer, and musician who traces his connections to Indian Country through consulting work with the Confederated Tribes & Bands of Yakama Nation in central Washington state as well as via his music and Missouri Cherokee heritage. His series of critiques of the U.S. mental health system’s checkered role with Native Americans for Indian Country Today (ICT) was well received and controversial. His new book, Coyote's Swing: A Memoir & Critique of Mental Hygiene in Native America, is currently pending
Dr. Walker is a liberation psychologist, writer, and musician who traces his connections to Indian Country through consulting work with the Confederated Tribes & Bands of Yakama Nation in central Washington state as well as via his music and Missouri Cherokee heritage. His series of critiques of the U.S. mental health system’s checkered role with Native Americans for Indian Country Today (ICT) was well received and controversial. His new book, Coyote's Swing: A Memoir & Critique of Mental Hygiene in Native America, is currently pending 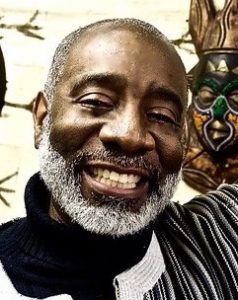 Dr. Washington is an African-Centered psychologist licensed in Florida and Washington, DC. He is a graduate of Grambling State University as well as Texas A&M University. He has taught/lectured at several colleges nationally and internationally. NBCUniversal/BEN, National Alliance to End Homelessness, Roland Martin, Essence and many other national and international organizations have sought his expertise on psychological matters. He is a Past President of the Association of Black Psychologists and is currently an Associate Professor and Head of the Sociology and Psychology at Grambling State University and he is the National Director of Black Marriage Day. As a Fulbright-Hays scholar Kevin (Mwata) researched the impact of socializing institutions on the healing or restructuring of post-apartheid South Africa (Azania). It was in South Africa where he researched Ubuntu and how it can inform mental health service delivery to people of African ancestry and others. Much of his work focuses on healing the psycho-spiritual wounds that are present within people as a result of Cultural and Historical Trauma. Mwata continues to develop healing paradigms for persons of African ancestry who have been impacted by Persistent Enslavement Systemic Trauma (PEST). He is the founder of Ubuntu Psychotherapy which is a culturally sensitive modality for mental health counseling and Psychotherapy for Black men and boys as well as Black/African families. He advances culturally-relevant trauma informed care and interventions to be utilized by psychotherapists, that are culturally inclusive and particularized to the healing of Black and brown people. Through his research and writing he seeks to assist people to live life with power, purpose and passion.
Dr. Washington is an African-Centered psychologist licensed in Florida and Washington, DC. He is a graduate of Grambling State University as well as Texas A&M University. He has taught/lectured at several colleges nationally and internationally. NBCUniversal/BEN, National Alliance to End Homelessness, Roland Martin, Essence and many other national and international organizations have sought his expertise on psychological matters. He is a Past President of the Association of Black Psychologists and is currently an Associate Professor and Head of the Sociology and Psychology at Grambling State University and he is the National Director of Black Marriage Day. As a Fulbright-Hays scholar Kevin (Mwata) researched the impact of socializing institutions on the healing or restructuring of post-apartheid South Africa (Azania). It was in South Africa where he researched Ubuntu and how it can inform mental health service delivery to people of African ancestry and others. Much of his work focuses on healing the psycho-spiritual wounds that are present within people as a result of Cultural and Historical Trauma. Mwata continues to develop healing paradigms for persons of African ancestry who have been impacted by Persistent Enslavement Systemic Trauma (PEST). He is the founder of Ubuntu Psychotherapy which is a culturally sensitive modality for mental health counseling and Psychotherapy for Black men and boys as well as Black/African families. He advances culturally-relevant trauma informed care and interventions to be utilized by psychotherapists, that are culturally inclusive and particularized to the healing of Black and brown people. Through his research and writing he seeks to assist people to live life with power, purpose and passion. Dr. Tarantolo is a psychiatrist, psychoanalyst, group therapist for over 40 years on Capitol Hill. He specializes in helping patients come off psychotropic drugs.
Dr. Tarantolo is a psychiatrist, psychoanalyst, group therapist for over 40 years on Capitol Hill. He specializes in helping patients come off psychotropic drugs. Dr. Grace Jackson is a board certified psychiatrist who graduated summa cum laude from California Lutheran University with a Bachelor of Arts in political science and a Bachelor of Science in biology, as well as a Master’s Degree in Public Administration. She earned her Medical Degree from the University of Colorado Health Sciences Center in 1996 and completed her internship and residency while in the U.S. Navy.
Dr. Grace Jackson is a board certified psychiatrist who graduated summa cum laude from California Lutheran University with a Bachelor of Arts in political science and a Bachelor of Science in biology, as well as a Master’s Degree in Public Administration. She earned her Medical Degree from the University of Colorado Health Sciences Center in 1996 and completed her internship and residency while in the U.S. Navy. MSgt Troy Drasher (USAF, ret)
MSgt Troy Drasher (USAF, ret) HM1(FMF) Shannon Book (USN, ret)
HM1(FMF) Shannon Book (USN, ret) Sgt Meeka McWilliams (USA, ret)
Sgt Meeka McWilliams (USA, ret)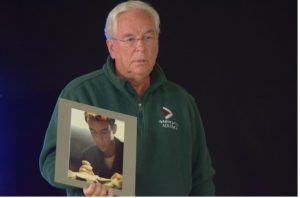 SPC4 David Rose (USA)
SPC4 David Rose (USA) LCpl Douglas Gresenz (USMC)
LCpl Douglas Gresenz (USMC) Jason Lott
Jason Lott
 Our dear friend and colleague, Paula J. Caplan, Ph.D., died on July 21, 2021 at her home in Rockville, Maryland. Paula was a tireless advocate for those who have been harmed by the conventional mental health industry, especially women and veterans. She has touched the lives of countless people and we can still hear the echoes of her forceful message.
Our dear friend and colleague, Paula J. Caplan, Ph.D., died on July 21, 2021 at her home in Rockville, Maryland. Paula was a tireless advocate for those who have been harmed by the conventional mental health industry, especially women and veterans. She has touched the lives of countless people and we can still hear the echoes of her forceful message. Chuck Ruby, Ph.D., Psychologist
Chuck Ruby, Ph.D., Psychologist

